A Comprehensive Guide to Incentive Programs in the Healthcare Landscape
Related Articles: A Comprehensive Guide to Incentive Programs in the Healthcare Landscape
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to A Comprehensive Guide to Incentive Programs in the Healthcare Landscape. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
A Comprehensive Guide to Incentive Programs in the Healthcare Landscape
In the ever-evolving healthcare landscape, optimizing resource allocation and achieving desired outcomes is paramount. Incentive programs, particularly those focused on improving healthcare quality and efficiency, have emerged as a crucial tool for achieving these objectives. These programs, often referred to as "value-based care" models, incentivize healthcare providers to prioritize patient well-being and deliver high-quality, cost-effective care. This article delves into the intricacies of incentive programs, exploring their various forms, benefits, and challenges, ultimately highlighting their critical role in shaping the future of healthcare.
Understanding Incentive Programs: A Framework for Transformation
Incentive programs in healthcare are designed to motivate providers to adopt specific behaviors or achieve predefined goals. They operate on the principle of aligning financial rewards with desired outcomes, fostering a shift from volume-based care to value-based care. This paradigm shift encourages providers to focus on improving patient health, reducing unnecessary procedures, and optimizing resource utilization.
Types of Incentive Programs: A Diverse Landscape
Incentive programs come in various forms, each tailored to specific goals and target populations. Some common types include:
- Pay-for-Performance (P4P): This model rewards providers for achieving predefined performance measures, such as improving patient satisfaction, reducing readmissions, or managing chronic conditions effectively.
- Shared Savings Programs: These programs incentivize providers to reduce healthcare costs while maintaining quality of care. Savings generated through cost-effective practices are shared between the provider and the payer.
- Bundled Payments: In this model, providers receive a fixed payment for a specific episode of care, such as a hip replacement or a heart attack. This incentivizes providers to manage costs and coordinate care effectively throughout the episode.
- Accountable Care Organizations (ACOs): ACOs are groups of healthcare providers who collaborate to provide coordinated care to a defined patient population. They are incentivized to improve quality and reduce costs, sharing in the financial benefits generated.
Benefits of Incentive Programs: A Catalyst for Change
The implementation of incentive programs has yielded significant benefits across the healthcare landscape:
- Improved Quality of Care: By rewarding providers for achieving specific quality metrics, incentive programs promote a focus on patient-centered care, leading to better health outcomes.
- Reduced Healthcare Costs: Programs that incentivize providers to reduce unnecessary procedures and optimize resource utilization contribute to lower overall healthcare spending.
- Enhanced Patient Satisfaction: By prioritizing patient well-being and providing high-quality care, incentive programs contribute to increased patient satisfaction and improved healthcare experiences.
- Increased Efficiency: Incentive programs foster innovation and efficiency within healthcare systems, encouraging providers to adopt new technologies and streamline processes.
- Enhanced Provider Collaboration: Programs that promote shared savings or bundled payments incentivize providers to collaborate effectively, improving care coordination and reducing fragmentation.
Challenges and Considerations: Navigating the Complexity
While incentive programs offer numerous benefits, they also present challenges that must be addressed effectively:
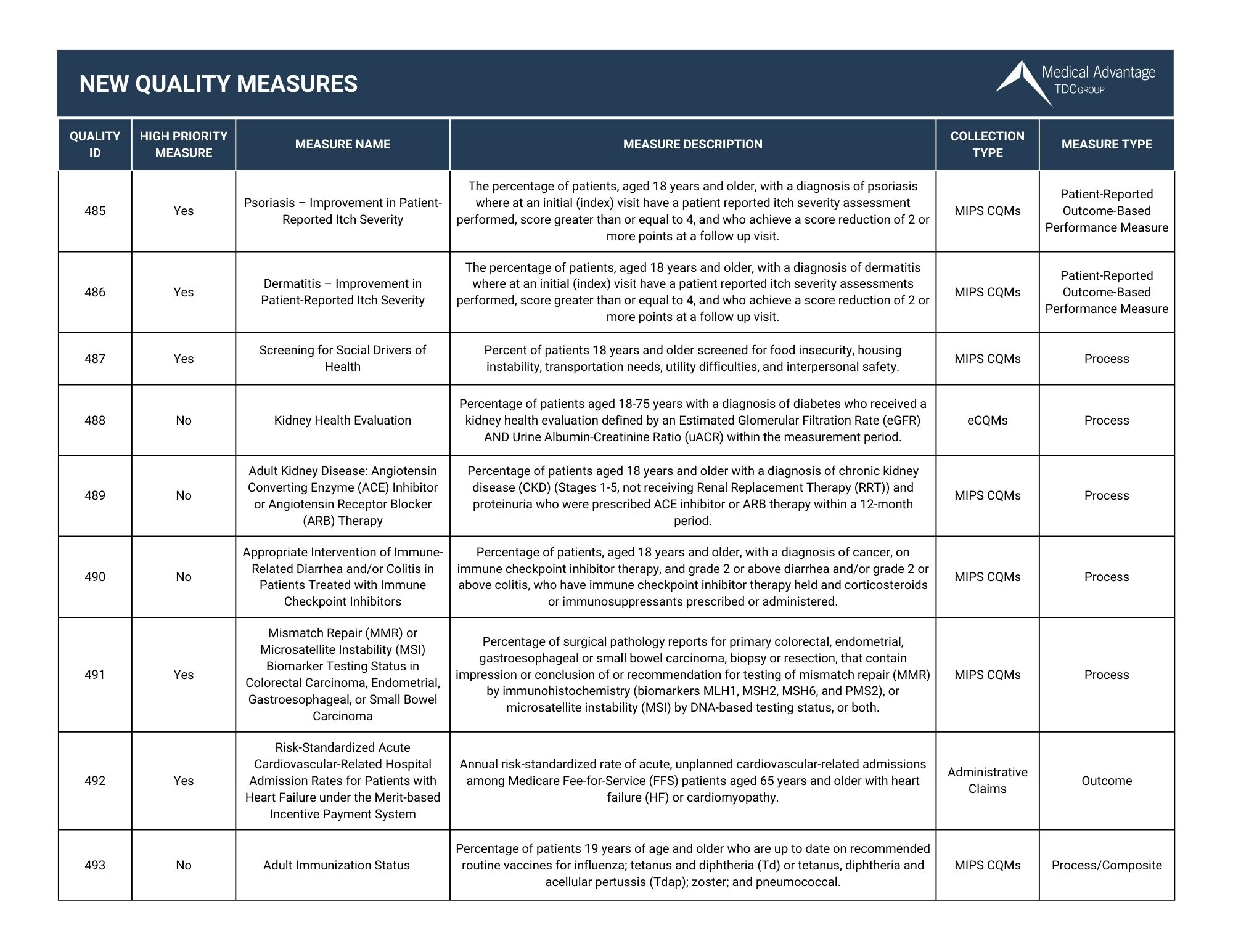
- Data Collection and Measurement: Accurate and reliable data collection is crucial for measuring performance and ensuring fair compensation. Establishing robust data infrastructure and standardized measures is essential.
- Complexity and Administrative Burden: Designing and implementing incentive programs can be complex and require significant administrative effort. Simplifying program structures and streamlining administrative processes can mitigate these challenges.
- Potential for Bias: Ensuring that incentive programs are designed and implemented fairly, without creating unintended biases or disincentivizing certain providers, is critical.
- Transparency and Accountability: Maintaining transparency in program design and implementation, ensuring accountability for performance, and providing clear communication to stakeholders are essential for building trust and ensuring program effectiveness.
FAQs Regarding Incentive Programs in Healthcare
1. What are the key performance indicators (KPIs) used in incentive programs?
KPIs vary depending on the specific program objectives. Common metrics include:
- Quality Measures: Patient satisfaction, readmission rates, mortality rates, adherence to clinical guidelines.
- Cost Measures: Total cost of care, cost per episode of care, utilization of services.
- Efficiency Measures: Timeliness of care, wait times, communication effectiveness.
2. How are incentive payments calculated?
Payment structures vary based on program design. Common approaches include:
- Performance-based payments: Payments are directly linked to achieving specific performance targets.
- Shared savings models: Providers share in the savings generated through cost-effective practices.
- Bundled payments: Providers receive a fixed payment for a specific episode of care.
3. What are the ethical considerations associated with incentive programs?
Ethical considerations include:
- Potential for conflicts of interest: Ensuring that incentive programs do not incentivize providers to prioritize financial gain over patient well-being.
- Equity and access to care: Ensuring that all patients have access to high-quality care, regardless of their ability to pay.
- Transparency and accountability: Maintaining transparency in program design and implementation and holding providers accountable for their performance.
4. How can incentive programs be effectively implemented?
Effective implementation involves:
- Clear program objectives and performance targets.
- Robust data collection and measurement systems.
- Transparent communication and stakeholder engagement.
- Regular program evaluation and adjustments.
Tips for Optimizing Incentive Programs
- Align program objectives with broader healthcare goals.
- Involve stakeholders in program design and implementation.
- Utilize data analytics to monitor performance and identify areas for improvement.
- Promote collaboration and knowledge sharing among providers.
- Continuously evaluate and refine program design based on evidence and feedback.
Conclusion: A Path Towards a More Efficient and Effective Healthcare System
Incentive programs have emerged as a powerful tool for transforming the healthcare landscape. By aligning financial incentives with desired outcomes, these programs promote a shift from volume-based care to value-based care, fostering a culture of quality, efficiency, and patient-centeredness. While challenges remain, ongoing efforts to refine program design, enhance data infrastructure, and address ethical considerations are essential for realizing the full potential of incentive programs in creating a more sustainable, equitable, and effective healthcare system.




Closure
Thus, we hope this article has provided valuable insights into A Comprehensive Guide to Incentive Programs in the Healthcare Landscape. We hope you find this article informative and beneficial. See you in our next article!